Fall Risks: A Step-by-Step Plan for Your Patients

Fall risks are a significant concern for many facilities. According to the Agency for Healthcare Research and Quality (AHRQ), approximately half of the 1.6 million residents in U.S. nursing facilities fall each year. Falls often have serious consequences, including:
- Reduced quality of life
- Decreased ability to function
- Serious injuries
- Increased risk of death
- Increased fear of falling
As more patients experience falls in a nursing home or rehabilitation setting, it has become increasingly important to implement a fall prevention program in your facility. There can be major consequences for facilities that do not implement a fall risk plan, including:
- Increased paperwork for staff
- Increased levels of care required for fallers
- Poor customer ratings
- Lawsuits
- High insurance premiums
While not all falls and injuries can be prevented, it is critical to have a process of assessment, intervention, and monitoring to minimize fall risks in your facility. Continue reading for a step-by-step plan to reduce and monitor falls in your facility.
Step 1: Fall Risk Assessment

A fall risk assessment includes several steps, including a symptom, history and medication review as well as tests and follow-up care.
Symptoms, History and Medication Review
As a healthcare provider, you should:
- Ask your patient to describe their previous falls, such as what caused the fall, what happened following the fall, and if they received medical treatment
- Ask about the patient’s activity level and ability to perform daily tasks
- Review your patient’s medication to see if any increase the patients fall risk
Tests and Follow-Up Care
Ensure your patients perform proper tests and follow up care. Assessments for fall risks should be conducted at least once a year.
- Check your patients for low blood pressure and heart palpitations
- Perform a physical exam using multiple tests
- Order lab results to check vitamin levels or to check for osteoporosis
Healthcare providers use these fall risk assessment tools to test their patients balance, strength and gait (pattern of walking):
- 30-Second Chair Stand Test: Your patient will sit in a chair with their arms crossed to prevent the patient from using their arms as support. Count the number of times they can stand up and sit down in 30 seconds.
- Four Stage Balance Test: The patient will hold four different positions for 10 seconds each. Positions vary in difficulty with the fourth one involving standing on one foot.
- Timed Up & Go (TUG): The patient will start by sitting in a chair with armrests. They will get up and walk 10 feet at their usual pace and return to the chair to sit down. If it takes the patient 12 seconds or more to prevent this exercise, they likely have a high fall risk.
- Cognitive Tests: You may perform a brief cognitive assessment to check any problems with thinking.
After completing a fall risk assessment, the healthcare provider may let your patient know whether they have a low or high risk of falling. They may recommend the patient to:
- Attend physical therapy to help gain strength & balance
- Install grab bars in their bathrooms
- Try group exercise classes geared towards older adults or individuals with balance issues
- Take vitamins if they are vitamin deficient
- Switch medications if any current medications cause a fall risk
- Use assistive devices
- See an eye doctor to correct any vision problems or conditions
- And more
Step 2: Individualized Exercise Programs
While it’s not possible to completely prevent a fall from occurring, exercises that focus on balance and strength training can reduce the risk of falling. A tailored exercise program should be developed to address the patient’s specific needs. Strength training can help improve:
- Muscle tone
- Flexibility
- Range of motion
Balance exercises can help patients improve:
- Gait pattern
- Stability
- Strengthen core muscles
- Posture
It is essential that the exercises performed are appropriate for the patient’s fitness level and health condition.
Step 3: Medication Review

Medications can sometimes cause dizziness or drowsiness, increasing the risk of falls. According to the National Library of Medicine, dizziness and vertigo are among the most common disorders in medicine, affecting approximately 20-30% of individuals.
A comprehensive medication review by the patient’s healthcare professional is crucial to identify any medications that might contribute to the patient’s fall risk. The healthcare professional may consider adjusting dosages or recommending alternative medications to help reduce or eliminate vertigo and dizziness.
Step 4: Living Space Safety Assessment
Falls often occur where the patient lives, making a safety assessment vital for fall risk patients. This assessment should focus on identifying and addressing potential hazards such as:
- Loose rugs
- Slippery floors
- Poorly lit areas
- Cluttered pathways
Cleaning the hazardous areas, installing grab bars in bathrooms, and using non-slip mats can help significantly reduce fall risks.
Step 5: Assistive Devices

Assistive devices may be necessary for fall risk patients. Some assistive devices that may help the patient remain steady are:
- Canes
- Crutches
- Walkers
- Rollators
- Knee scooters
- Wheelchairs
- And more
These devices may be effective for patients during their daily activities. However, they may need more protection from falls during exercise and physical therapy. The Solo-Step Overhead Track & Harness System is an effective assistive device designed to prevent falls during physical therapy.
The Solo-Step Overhead Track System consists of a ceiling mounted aluminum rail, attached to a harness. The patient would be strapped into the harness, completely protecting them from slips, trips and falls. The Solo-Step allows your patients to:
- Overcome their fear of falling
- Gain confidence
- Challenge themselves during physical therapy
- Be safe from slips, trips, and falls
If you’d like to learn more about the Solo-Step Overhead Track System, click the button below!
Step 6: Vision Check-Up
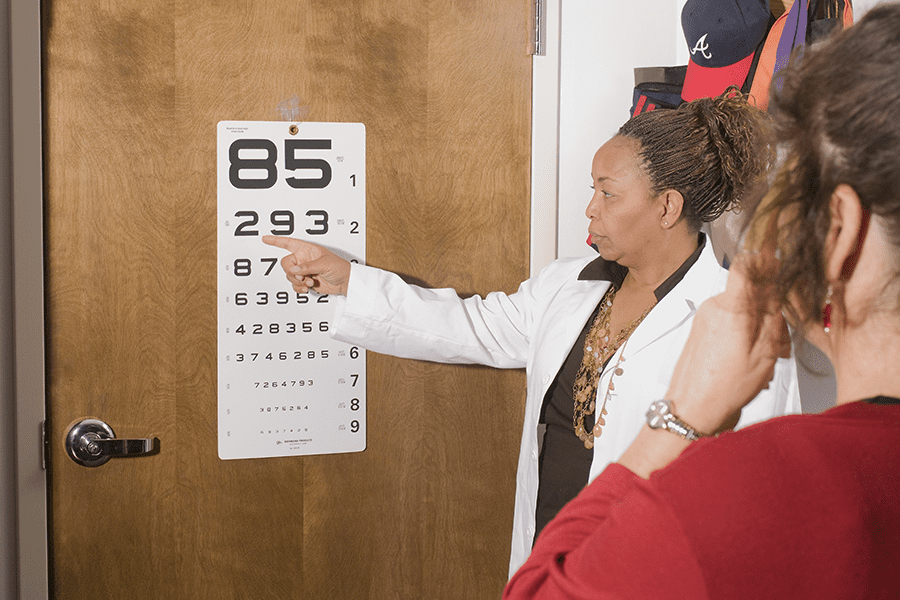
Vision plays a significant role in balance. According to the Neuro-Optometric Rehabilitation Association, approximately twenty percent of the nerve fibers from the eyes interact with the vestibular system. There are many visual dysfunctions that can cause, or associate with dizziness and balance problems.
Regular eye exams should be scheduled to correct any vision problems promptly. Wearing appropriate eyeglasses or using prescribed aids can improve safety and decrease fall risks for your patients.
Step 7: Nutrition & Hydration
Maintaining a well-balanced diet and staying hydrated is crucial for overall health and reducing fall risk. Adequate nutrition ensures your patient has stronger bones and muscles, reducing the chance of falls.
Staying hydrated is an essential component of fall prevention. Proper hydration can help prevent dizziness and confusion, while also helping your muscles heal and stay strong.
Step 8: Regular Follow-Ups

Fall risk patients should have regular follow-up appointments with their healthcare providers to:
- Monitor progress
- Update exercise & therapy plans
- Reassess risk factors
- Update their medications
- Check their vision
Regularly checking up with patients and reminding them of scheduled appointments is important for the health and safety of fall risk patients.
By following this step-by-step plan, fall risk patients can take proactive measures to reduce their risk of falls, enhance their independence, and maintain a higher quality of life. Every patient’s needs are unique, so personalized care is key to achieve the best outcomes for each of your patients. With the support of healthcare professionals, family members, and a safe therapy/living environment, fall risk patients can navigate their daily lives while minimizing the risk of falls.
For more Solo-Step blogs, click here!